What is Antimicrobial Resistance?
Antimicrobial resistance (AMR) occurs when microorganisms such as bacteria, viruses, fungi and some parasites develop mechanisms to resist being killed by antimicrobial agents such as antibiotics1. Infections thus persist and may spread to others2.
Find facts on Antimicrobial Resistance here.
[1] Joint External Evaluation of IHR Core Capabilities, Singapore
[2] Centers for Disease Control and Prevention (CDC)
Why is AMR a Concern?
Antimicrobial resistance presents a major threat to global health. With the gradual and increasing development of resistance to antimicrobial agents, crucial medicines lose their ability to effectively treat infections and threaten to reverse benefits achieved as a result of the advancement of science and medicine3. The UN Interagency Coordinating Group on Antimicrobial Resistance (IACG) warns that drug-resistant diseases could lead to a projected 10 million deaths globally each year by 20504 and highlights the projected economic strain from the impact of dealing with prolonged hospitalisation stays and increased morbidity as a result of ineffective medicines.
AMR may affect anyone at any stage of life2 and is evolving at a rate that outpaces the development of new antimicrobial agents to deal with them. With increased global connectivity through trade and travel, AMR has the potential to spread and poses a threat to all countries.
[3] National Strategic Action Plan (NSAP) on Antimicrobial Resistance, Singapore
[4]World Health Organisation (WHO) No Time to Wait: Securing the Future from Drug-Resistant Infections. Report to the Secretary General of the United Nations
What Can We Do to Fight Antimicrobial Resistance?
There is a need to tackle the drivers of AMR and reduce the emergence and prevent the spread of drug-resistant organisms. AMR is accelerated by human activities such as the overuse and misuse of antimicrobials in humans, plants and animals, the spread of infections and the contamination of the environment5.
In May 2015, the World Health Assembly endorsed a Global Action Plan to set out key priority areas to combat the urgency for AMR. The objectives of the Global Action Plan include improving AMR awareness, optimising the use of antimicrobials, strengthening surveillance and research, and reducing infections.
Read more about the WHO Global Action Plan here.
The UN Inter-Agency Coordinating Group (IACG) recommends urgent action by all stakeholders in recognition of the interlinked human, animal, food and environment sectors. A 'One Health' approach is particularly useful in combating AMR as cross-sector collaboration is crucial in addressing challenges posed by AMR6 and is highlighted in Singapore's National Strategic Action Plan (NSAP). The NSAP brings together agencies including the Ministry of Health (MOH), Animal and Veterinary Service (NParks/AVS), National Environment Agency (NEA), Singapore Food Agency (SFA) and PUB, Singapore's National Water Agency, to facilitate and coordinate AMR efforts across human, environmental, food and animal sectors.
In September 2018, the Antimicrobial Resistance Coordinating Office (AMRCO) was established as a coordinating body to facilitate the implementation and monitoring of the NSAP, coordinate AMR efforts across different sectors and serve as secretariat for national AMR committees.
[5] World Health Organisation (WHO) Framework for Accelerating Action to Fight Antimicrobial Resistance in the Western Pacific Region
[6] National Food Institute, Technical University of Denmark (DTU) One Health Integration in Surveillance
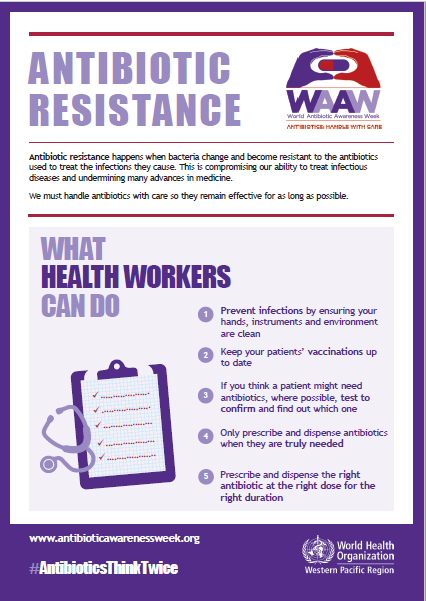
How Can Healthcare Professionals Play Their Part?
Judicious prescribing of antibiotics plays a key role in minimising the risk of misuse. Appropriate infection prevention and control measures will further reduce the risk of the spread of antimicrobial-resistant organisms. It is imperative for healthcare professionals to prioritise educating patients on the importance of appropriate use of antibiotics and to receive recommended vaccines to prevent the spread of infections.
Source: World Health Organisation
Find Infection Control Guidelines for Healthcare Facilities here.
National Surgical Antibiotic Prophylaxis Guideline
(Singapore)
The National Surgical
Antibiotic Prophylaxis Guideline (Singapore) provides evidence-based
recommendations for the rational use of antibiotic prophylaxis, including
recommended agent(s), dose, timing and duration for adult patients undergoing
elective clean or clean-contaminated surgeries. This guideline aims to align
best practices nationally and provide a framework for audit and surveillance.
The establishment of the national SAP guideline for hospitals in Singapore may
reduce the rate of surgical site infections, while also reducing adverse events
from prolonged duration of surgical prophylaxis.
The Guideline was developed through
multidisciplinary collaborations of the National Antimicrobial Stewardship
Expert Panel (NASEP) National SAP Guideline Development Workgroup, comprising
Infectious Disease (ID) physicians, ID and/or antimicrobial stewardship-trained
pharmacists, surgeons, and anaesthesiologists; and endorsed by NCID and the
Chapter of ID Physicians, College of Physicians, College of Anaesthesiologists
and College of Surgeons under the Academy of Medicine, Singapore.